It has been 12 years since the Affordable Care Act (ACA) was passed in 2010. The law is known more for health insurance reforms, but it also brought into the limelight the urgent call for value-based healthcare delivery. With ACA, the goal is to effectively shift from a fee-for-service to a value-based care model which focuses more on overall wellness and prevention. In truth, the very idea of value-based care was introduced way back in 2006, but at the time, did not gain traction as many providers were unable to focus on “well care” because “sick care” demanded most of their time, energy, and resources.
What is value-based care?
Value-based care is a proactive concept focused on patient outcomes and how providers can effectively enhance the quality of care with specific measurable results like avoiding hospitalizations or averting a medical crisis due to complications.
Providers under the value-based care model will receive reimbursements based on the quality of care they provide and incentives on their ability to add efficiency and effectiveness to their care. This type of reimbursement opens to providers an alternative and potentially lucrative supplement to traditional fee-for-service payments.
The Center for Medicare and Medicaid Services (CMS) has pushed for a range of value-based care delivery models like the Medicare Shared Savings Program, Next Generation Accountable Care Organization (ACO) model, and the Pioneer ACO model. Meanwhile, private payers also have done the same with similar models of accountable value-based care. All these models reward providers for assisting their patients to lead healthier and quality lives. A healthier patient reduces healthcare costs for everyone.
What healthcare solutions promote value-based care?
Medicare has introduced Chronic Care Management (CCM) in 2015 and after three years, Remote Patient Monitoring (RPM) in 2018.
CCM is one of many value-based care initiatives by CMS to aid overwhelmed practices, which simply cannot carry out their own value-based solution for their chronic care patients considered to be the most at high-risk and high-cost patient population. Meanwhile, RPM is one of the strategies of CMS to ensure patients have access to virtual care services, especially for isolated or remote patient populations.
CCM continues the care in-between office visits through a comprehensive care plan, medication adherence, and care coordination between specialists and primary care providers. Medicare patients with two or more chronic conditions can be eligible to participate in a CCM program. CMS provides an incentive every month to providers for each enrolled CCM patient. The reimbursements will translate into hundreds of dollars per year for each CCM beneficiary, adding to that the fee-for-service and shared savings, making it a lucrative endeavor for a practice.
RPM uses digital technology with remote devices to capture and transmit patient data for clinicians to ascertain the overall condition of their patients. Abnormal readings can be easily detected and used to change the trajectory of care. Like CCM, CMS also offers incentives to providers when they set up and educate patients, read and interpret patient data, and make the necessary interventions.
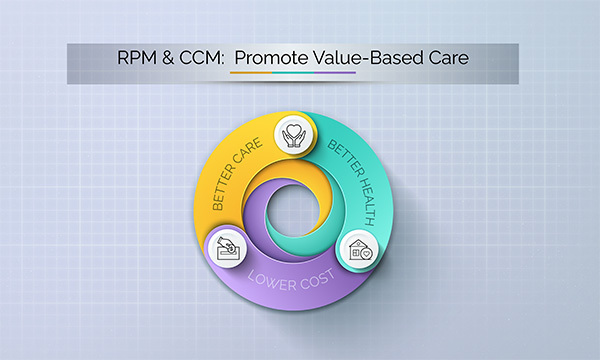
Through CCM and RPM, CMS is pushing for quality not the quantity of services typical of the traditional fee-for-service reimbursement model. Value-based care has a triple aim of enhancing patient care, strengthening strategies for population health management, and reducing costs.
So how do CCM and RPM promote value-based care?
1. Enable timely and appropriate clinical interventions
Both CCM and RPM provide the infrastructure for the right patient intervention. For instance, CCM requires a remote care nurse to engage with the patients telephonically every month. This routine monitoring allows for easy detection that could prevent escalation or a medical crisis. On the other hand, RPM provides real-time data to support clinicians in their clinical decision-making. The extra layer of care provided by both CCM and RPM promotes preventative care with the right and timely clinical interventions.
2. Provide the framework to optimize care
CCM and RPM provide the framework for value-based care having the same skills and assets required to ensure a better quality of care for patients. Both programs are used in disease management through care instructions and review of patient data. The clinical time is not limited or restricted to the schedule of doctors and the length of the patient queue outside so a broader scope of issues can be resolved, not just one specific complaint. Enrolled patients feel they are truly cared for with an additional layer of support, which leads to improved patient engagement, accountability, and satisfaction. In addition, the technologies used provide better access to healthcare as seen during the pandemic with chronic care patients relying more on telehealth and avoiding doctor’s offices entirely.
3. Gather clinical data needed for compliance
CCM and RPM play an important role in formalizing value-based care by assisting primary care providers to perform their core competencies without the burden of ensuring compliance and avoiding penalties. On many occasions, providers are compelled to gather and report more data, spending hours facing their screens ticking off boxes. Care nurses can engage the patients, foster trust, and obtain the needed clinical data. Moreover, RPM devices are fully configured for easy use and data is transmitted even without user intervention. Both CCM and RPM provide the personalized support chronic care patients need while helping primary care providers manage their chronic care.
4. Significantly reduce costs
The very essence of value-based care is to reduce costs because chronic care is exacting a heavy toll on the healthcare industry. CCM and RPM promote preventative care thereby translating into substantial savings for patients, providers, and payers alike. By being proactive, a patient’s condition does not escalate or require hospitalizations. Moreover, chronic care patients are able to receive a higher quality of care without leaving the comfort of their own homes.
5. Empower primary care
Primary care providers are the first line of defense for being in charge of care maintenance, prevention, and patients to avoid hospitalizations. Though they contribute little to overall healthcare spending, they can drastically reduce downstream patient spending by 90%. For a value-based care model to be effective, primary care should be accessible and efficient. Primary care providers must have the capacity to provide patient-centered care, which CCM and RPM are designed for. These virtual care solutions empower primary care physician practices to innovate and optimize their patient care while offering an opportunity to earn a new revenue stream.
Why does it make sense for a certain aspect of value-based care to be outsourced?
Providers are already overwhelmed with treating their sick and aging patients, let alone complying with CMS mandates. They cannot be expected to start their own CCM and RPM programs without the additional administrative and operational burdens. Some have attempted and were successful to a degree, but were not able to overcome inherent obstacles as patient volume increased. While others have balked because of the heavy investment needed to set up the tools and infrastructure as well as the technology to run an effective combination of CCM and RPM programs. In addition, many practices simply do not have the capabilities needed to navigate the intricate regulatory requirements to maximize their earnings.
Ascent Care Partners (ACP) offers turnkey CCM and RPM programs as a full service, with no upfront cost or risk to the practice. ACP aims to help primary care physicians’ practice realize a much-deserved revenue without increased overhead. Leveraging years of working in the healthcare industry and making billing reports, ACP can optimize your patient care and help your practice grow financially.